Occupational Safety of Health Workers From COVID-19 in Laparoscopic Surgery

Management Protocol For COVID-19 Pandemic
This work seeks to specify and analyze the risk of viral contamination during laparoscopy in the context of the Covid-19 pandemic of health professionals. As well as the means of protection and prevention necessary in clinical practice. Ethicon Laparoscopic Trainer.
Laparoscopic Training simulation with Ethicon Laparoscopic Trainer is a practical choice.
The COVID-19 pandemic has changed the management protocols of the different areas and surgical practices of health institutions in the world. The nations generally impacted by the illness alarmingly affect the quantity of tainted and expired by Covid-19 among wellbeing laborers.
Surgical Smoke Cause Of COVID-19 Pandemic
Currently, the pandemic caused by SARS-CoV-2 reports that 80% of patients have mild symptoms or are asymptomatic, behaving as potential carriers and transmitters. Conventional routes of transmission (droplets, aerosols, and direct contact) are the main mechanisms involved in contagion, although the virus also finds in the gastrointestinal tract, saliva, and urine. The Center for Disease Control and Prevention mentions the transmission of the virus during risky medical procedures as a major exposure. In addition, the surgical team faces another potential route of spread through surgical smoke.
Health Workers Infected With COVID-19
By early 2020, reported more than 3,300 health workers infected with COVID-19, of whom at least 22 have died. On the other hand, more than 20% of those infected correspond to medical personnel and deaths reached more than 50 health workers for the same period. As of March 2020, the pandemic had spread throughout the world with more than 750,000 confirmed cases, including more than 36,000 deaths.
Currently, the world reports more than 113 million infected and 2.4 million deaths. On April 8, 2021, a total of 2,468,236 cases reports, of which 53,788 cases correspond to health personnel; 64,524 patients have died, 251 are doctors and nurses.
Safety Of Minimally Invasive Surgeries From COVID-19
Currently, the number of nosocomial infections attributed to the laparoscopic surgery process is unknown. However, international scientific societies debate the safety of minimally invasive surgeries for fear of virus transmission. Although information on it is scarce and recommendations focus on controlling aerosolization.
Methods
A narrative review carries out through a search in the databases. To investigate, depict and talk about the aerosolization avoidance measures and the methodology of Covid-19 patients in laparoscopic medical procedure. Considering the theoretical points of view from the different types of information according to the evidence.
Occupational Safety of Viral Transmission
The keywords and/or search heading according to the MeSh terms were: Covid-19, SARS-CoV-2, occupational safety, occupational exposure, laparoscopic surgery, and viral transmission. In the selection process, all original articles with recommendations of a high degree of evidence, published in English, includes. prioritizing those that analyze safety measures and aerosol management in patients with a confirmed diagnosis of SARS-CoV-2 undergoing laparoscopic surgery.
The review of the texts carries out by all the researchers, the articles select under 3 pre-established thematic areas:
- Risk of viral contamination,
- Prevention of aerosol exposure,
- Preoperative, intraoperative, and
- Postoperative management of infected patients in laparoscopic surgery.
A total of 30 articles reviews in which the main objective was to describe the practice of laparoscopic surgery under the COVID-19 pandemic, since they referred to the pre-established thematic areas and served for the development of this review. For minimally invasive surgery technique, many of them have not received practical training with simulators resembling Ethicon Laparoscopic Trainer.
Preoperative Management
Once the risk and benefit of takes to open or minimally invasive surgery evaluates. The availability of the operating room with qualified and trained human personnel verifies to reduce the risk of transmission to health personnel. Define a hospital route dedicated only to the transport of patients with Covid-19.
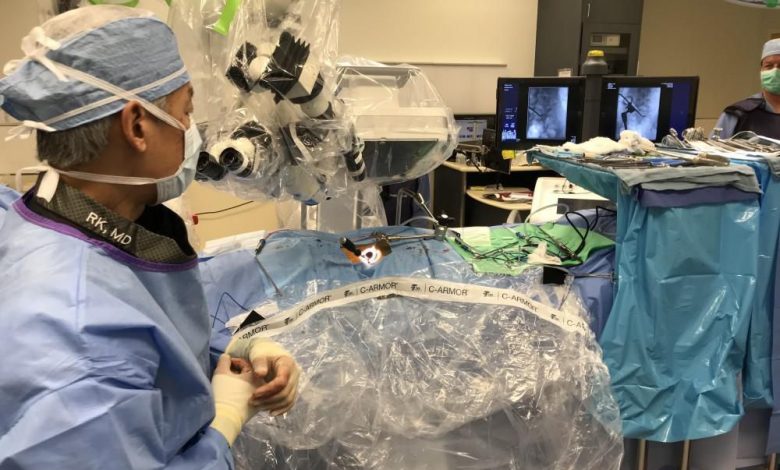
Facilitate Cleaning Personnel and Equipment
Involve the least number of health personnel and register them to facilitate follow-up and contact. Use all recommended personal protection measures for infection prevention. Restrict the movement of personnel in and out of the operating room. Anesthesia equipment, computers, desks, and necessary machines covers with plastic wrap to prevent contamination and facilitate cleaning. Ethicon Laparoscopic Trainer.
In general, several strategies use in operating rooms to reduce risks:
- Including negative pressure room ventilation,
- Avoiding cross-contamination between rooms,
- Changing the air in the operating room at least 12 times per minute and
- In ideal conditions 25 times per minute,
- Minimize time and exposure during intubation using N95 mask or higher protection face masks,
- As well as smoke evacuation systems.
Concern raises about N95 masks as they filter particles larger than 0.3 µm, given the small size of particles generated by electrocautery and ultrasonic scalpel; and the variable size between 0.06 to 0.14 µm of the SARS-CoV-2 molecules.
Conclusion
Personnel specialized in airway management have a higher risk of contagion by directly exposes to the aerosolization of the virus. This leads to considering the probability of postponing or restricting procedures due to limited resources and/or patient conditions that increase the risk of death, given that the usual surgical techniques generate more aerosols. This narrative review articles.
For more information visit our website: www.gerati.com




